< Back to Publications & Resources
Mitigating Risks Associated with Improper Performance
This article was originally published in MLMIC’s Million Dollar Claims Report.
Improper performance is an allegation made any time the anticipated outcome does not meet the expectations defined by the patient. A MLMIC analysis indicates that over two of every five (42%) claims brought against an insured alleged improper performance. This is seen most frequently in Surgery and in Obstetrics, for example, when complications arise during labor and delivery.
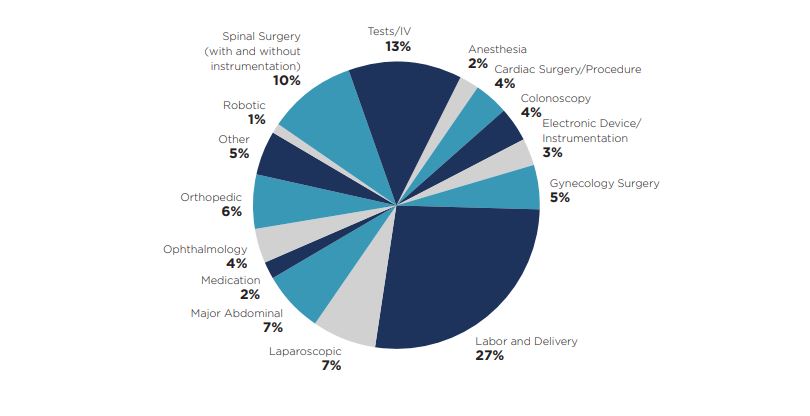
Improper Performance: A Breakdown by Procedure/Service
A closer look at the chief medical factor of improper performance shows that multiple specialties are involved, and different types of procedures are triggering lawsuits. For example, in a surgical specialty, improper performance may be alleged during the operative consultation, the operative procedure itself, the management of a patient in the Post Anesthesia Care Unit immediately after surgery, or during the care rendered prior to discharge from the floor or ambulatory surgical center. Nearly four in 10 (39%) of our files reviewed involved a surgical procedure. Examples include:
• a laparoscopic procedure that required conversion to an open procedure (e.g., to repair a bowel perforation);
• a spinal fusion performed with or without instrumentation (e.g., resulting in nerve damage); and
• an orthopedic procedure (e.g., a total knee replacement with postoperative sepsis, requiring joint removal and subsequent amputation above the knee).
In our review of closed claims, the specialty most often associated with improper performance was Obstetrics/Gynecology, which was cited in almost one-third (27%) of all files reviewed. The most common associated factor was labor and delivery. For example, an allegation of improper performance was made when a physician had to use maneuvers during a vaginal delivery for which the patient was not prepared; or when complications arose during the performance of a Cesarean section, exposing both mother and baby to a higher level of risk for injury.
At 13%, tests and intravenous therapy was the second largest category of claims in improper performance. These tests and therapies include instances such as the insertion of a central venous line for monitoring in an intensive care unit; or the insertion of a Broviac catheter for the administration of long-term therapies, such as chemotherapy; or a diagnostic bronchoscopy. In these cases, there was an expectation for each test or intravenous placement, which was not met, leading to allegations involving the informed consent process and lack of documentation in the medical record.
Informed Consent
When filing a claim or suit, a plaintiff attorney may also allege a lack of informed consent. In certain instances, such as during a routine physical examination or in a medical emergency where the delay in lifesaving care will cause harm, consent between the doctor and the patient is implied. However, for invasive tests and surgical procedures, informed consent must be obtained.
While there is a specific form to be completed and signed after an informed consent discussion between the doctor and the patient, there must also be reasonable documentation in the medical record that provides an accounting of the discussion. Informed consent is a nondelegable duty that rests with the physician who will be performing the test or procedure.
The discussion must include:
• Risks and benefits of the test/procedure
• Alternatives to the proposed treatment/procedure
• Risk of the alternative options
• Option of no treatment
• Time for questions and answers
• Consent to proceed with the proposed therapy
Policyholders are encouraged to review MLMIC’s Million Dollar Claims Report and risk management tips to help physicians and healthcare organizations improve patient care and, ultimately, reduce the number and severity of claims.



